Recent advancements in Alzheimer’s research have unveiled a groundbreaking approach known as TIM-3 Alzheimer’s treatment, leveraging the interactions of the immune system with brain cells to combat disease progression. This innovative method involves targeting the TIM-3 checkpoint molecule, which has been shown to inhibit microglia from effectively clearing amyloid plaques associated with Alzheimer’s. By blocking TIM-3, researchers have discovered that microglial function can be restored, enabling these brain immune cells to eliminate the harmful plaques and potentially improve memory performance in experimental models. This promising research not only highlights the implications of the immune system in Alzheimer’s but also offers a unique perspective on how cancer treatment strategies can be repurposed for neurodegenerative diseases. As scientists continue to explore the link between TIM-3 and cognitive decline, the opportunity for effective Alzheimer’s therapies that harness the immune response is rapidly evolving.
In the quest for effective Alzheimer’s solutions, the TIM-3 approach stands out as a pivotal strategy drawing on immune modulation principles. By focusing on the TIM-3 molecule and its impact on brain immune cells, known as microglia, researchers aim to enhance the clearance of neurotoxic plaques that contribute to dementia. This therapeutic avenue exemplifies the confluence of cancer treatment methodologies and neurobiology, opening new pathways for addressing cognitive impairment in Alzheimer’s patients. Recent studies focus on how altering the behavior of microglial cells may improve memory functions, ultimately reshaping the landscape of Alzheimer’s treatment options. As scientists delve deeper into these immune-related mechanisms, the potential for transformative therapies that can mitigate Alzheimer’s progression becomes increasingly tangible.
Understanding TIM-3 in Alzheimer’s Disease Treatment
The role of the TIM-3 molecule in Alzheimer’s disease (AD) represents a breakthrough in understanding the disease’s mechanisms. TIM-3, an immune checkpoint molecule, is critical for regulating the immune response in the brain. Recent research indicates that TIM-3 may contribute to the pathology of late-onset Alzheimer’s by inhibiting microglial cells from effectively clearing amyloid plaques. By interrupting this inhibitory signaling, researchers have observed improved cognitive function in mouse models. This opens up new avenues for Alzheimer’s treatment strategies targeting TIM-3.
This exciting research highlights the dual role of TIM-3 as both a protector and a potential impediment in Alzheimer’s disease. While the molecule helps maintain immune system balance, its overexpression in microglia can inhibit their ability to address plaque accumulation, a hallmark of Alzheimer’s pathology. Therapeutic strategies that involve blocking or deleting TIM-3 expression may enhance microglial activation and their plaque-clearing abilities, ultimately aiming to restore cognitive functions in affected individuals.
The Relationship Between Microglia Function and Alzheimer’s
Microglia, the brain’s resident immune cells, play a pivotal role in maintaining neural health and responding to pathologies such as Alzheimer’s disease. In a healthy brain, microglia continuously survey their environment, pruning synapses and clearing debris, a function that is crucial in forming and maintaining memories. However, in the context of AD, the microglial response becomes dysfunctional due to the increased expression of immune checkpoint molecules like TIM-3, leading to impaired clearance of toxic amyloid beta plaques.
The findings underscore the implications of microglial dysfunction in Alzheimer’s and highlight potential intervention strategies aimed at rejuvenating these immune cells. By understanding the signaling pathways that inhibit microglial activity, researchers can consider approaches to stimulate their plaque-clearing functions, possibly mitigating the cognitive decline associated with Alzheimer’s pathology. Enhanced microglial activity could potentially restore memory functions that are compromised in Alzheimer’s disease.
In Alzheimer’s research, understanding the intricate relationship between microglia and immune checkpoint molecules is essential for developing effective therapies. The need to balance the protective and detrimental roles of microglia will be crucial as scientists explore innovative treatment strategies targeting these immune cells.
Cancer Treatment Strategies Applied to Alzheimer’s Research
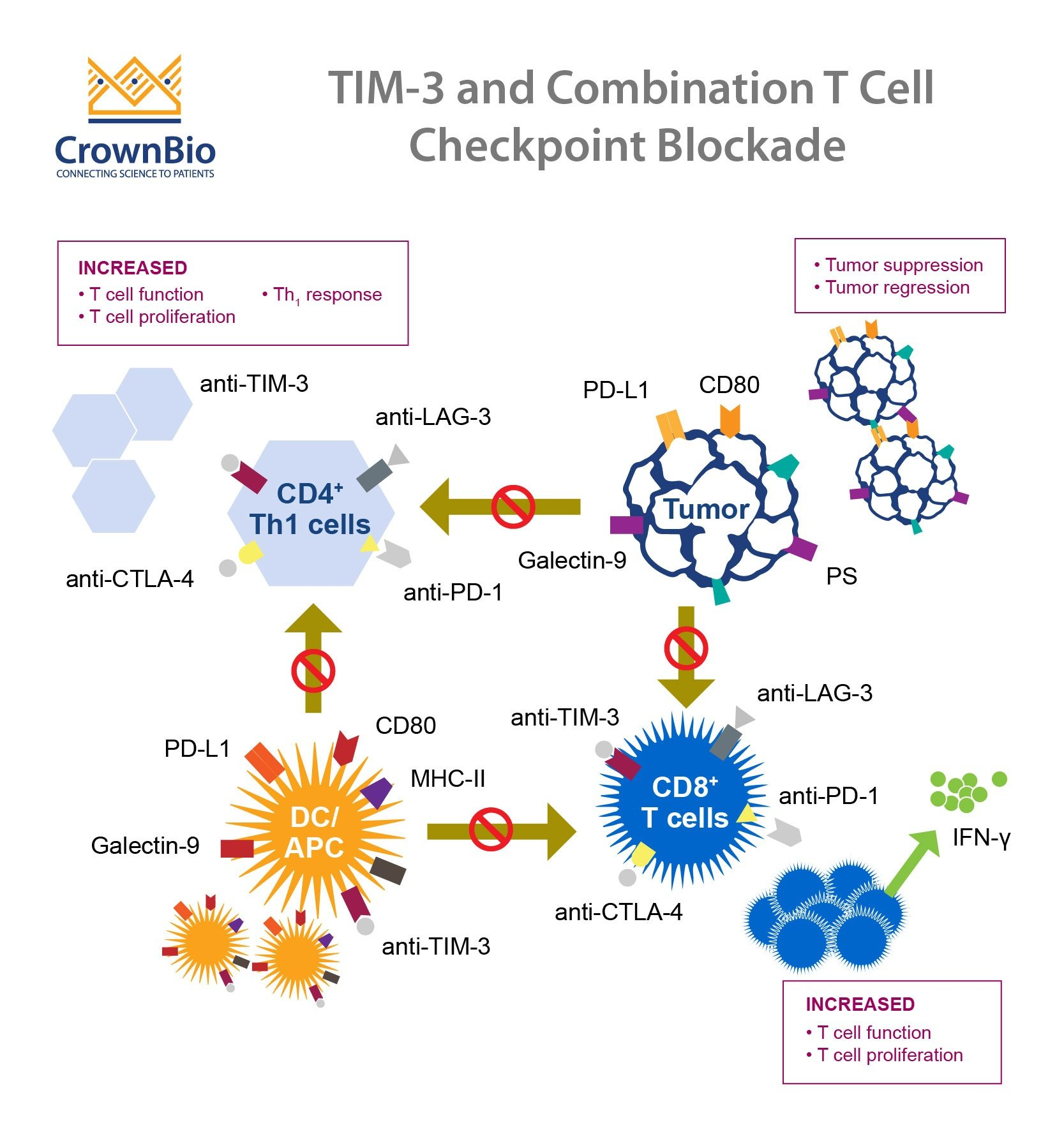
The innovative approach of utilizing cancer treatment strategies for Alzheimer’s disease illustrates a fascinating intersection between oncology and neurology. In cancer, checkpoint inhibitors have shown remarkable success in reviving the immune response against tumor cells. Similarly, the findings related to TIM-3 in Alzheimer’s disease suggest that modifying immune checkpoint activities could catalyze a neuroprotective response and enhance cognitive resilience in Alzheimer’s patients. This highlight paves the way for repurposing existing therapies designed for cancer treatment for neurological conditions.
As researchers explore the implications of immune checkpoint modulation, they draw parallels between the mechanisms of immune evasion in cancer and those seen in Alzheimer’s disease. The therapeutic potential of anti-TIM-3 antibodies presents an exciting frontier in Alzheimer’s research, offering hope for strategies that can enhance neuron health while lowering plaque accumulation. By leveraging knowledge from cancer research, scientists are better equipped to formulate novel treatments that may ultimately alter the course of Alzheimer’s disease.
The Promise of TIM-3 Therapies for Cognitive Restoration
Exploring TIM-3’s potential in cognitive restoration marks a significant development in Alzheimer’s treatment strategies. The ability to manipulate TIM-3’s inhibitory signaling could enable the revival of microglial functions vital for clearing amyloid plaques. As research progresses, the goal is to transition findings from mouse models to human applications, potentially transforming the landscape of Alzheimer’s treatment. This research not only aims to mitigate cognitive impairment but also enhances the overall quality of life for individuals affected by this debilitating disease.
Current advancements suggest that TIM-3 therapies could take the form of monoclonal antibodies or small molecules capable of inhibiting TIM-3’s function. As these therapeutic agents undergo preclinical evaluations, the scientific community remains hopeful that similar approaches utilized in cancer immunotherapy will lead to effective Alzheimer’s interventions. The promise of TIM-3 targeted strategies could herald a new era of actionable treatment protocols in the fight against Alzheimer’s disease.
Exploring the Genetic Link of TIM-3 to Alzheimer’s Risk
The genetic exploration of TIM-3 in relation to Alzheimer’s disease risk factors underscores the complexity of this neurodegenerative condition. A notable polymorphism in the HAVCR2 gene linked to TIM-3 expression has been implicated in increased susceptibility to late-onset Alzheimer’s. Understanding this genetic connection offers valuable insights into the etiology of Alzheimer’s disease and highlights the potential for genetic profiling in identifying individuals at risk. Such advancements may lead to more personalized treatment approaches.
Furthermore, investigating the link between genetic markers like TIM-3 and immune responses may aid researchers in developing strategies to modulate immune pathways effectively. Genetic studies on TIM-3 can provide critical information about the mechanisms by which immune dysfunction contributes to Alzheimer’s progression, allowing targeted interventions aimed at mitigating these effects. This level of genetic understanding could also enhance clinical trials by identifying suitable candidates for innovative therapies.
The Role of Immune System in Alzheimer’s Progression
The immune system’s involvement in Alzheimer’s progression has garnered significant attention in contemporary research. The traditional view of Alzheimer’s primarily as a neurodegenerative disorder is shifting towards a more nuanced understanding that includes immune system contributions. Factors such as chronic inflammation and the failure of immune cells to clear pathogenic proteins from the brain are emerging as focal points in Alzheimer’s pathology. This paradigm shift emphasizes the potential for targeting the immune system to alter disease trajectories.
Research indicates that microglia, the immune cells responsible for brain maintenance, become dysfunctional in Alzheimer’s, leading to increased accumulation of plaques and neuroinflammation. Understanding the immune system’s intricate role in Alzheimer’s not only opens pathways for novel therapeutic strategies but also changes the narrative surrounding the disease. By addressing immune dysfunction, researchers aim to create comprehensive treatment modalities that could have a profound impact on improving cognitive outcomes and slowing disease progression.
Investigating TIM-3 and Microglia in Alzheimer’s Research
Investigating the interplay between TIM-3 and microglia provides critical insights into the underlying mechanisms of Alzheimer’s disease. TIM-3’s role as an immune checkpoint prevents microglia from effectively engaging amyloid plaques, which are toxic to neurons. This inhibition leads to accumulated plaques in the brain, contributing to the cognitive decline characteristic of Alzheimer’s disease. Understanding how microglia respond to TIM-3 signaling underpins the potential for innovative therapeutic strategies aimed at unlocking their plaque-clearing function.
Through ongoing research, scientists are beginning to uncover the pathways by which TIM-3 influences microglial behavior in the context of Alzheimer’s. The focus is on delineating how altering TIM-3 expression or function can reinvigorate microglial activity, paving the way for treatments that could target this cellular dysfunction directly. By harnessing the inherent abilities of microglia and addressing their impediments, there is a tangible potential to develop effective therapies that could transform the prognosis for Alzheimer’s disease patients.
Challenges and Future Directions in Alzheimer’s Research
Despite promising developments in targeting TIM-3 for Alzheimer’s therapy, significant challenges remain in translating these findings from mouse models to human patients. The intricate biology of human Alzheimer’s disease introduces variables that are not always replicable in preclinical studies. Moreover, issues such as the blood-brain barrier’s permeability to therapeutic agents need to be addressed before these strategies can be safely and effectively implemented in clinical settings.
Future research will need to focus on the long-term effects of TIM-3 modulation and the potential for adverse outcomes caused by altering immune responses in the brain. Collaborative efforts between immunologists and neuroscientists will be vital in creating comprehensive treatment regimens that effectively address both Alzheimer’s pathology and cognitive decline. As advancements in technology and methodology continue, the hope is that effective TIM-3-based therapies will emerge, reshaping the landscape of Alzheimer’s disease treatment.
The Interconnection of Alzheimer’s Research and Immunology
The interconnection of Alzheimer’s research and immunology is becoming an increasingly vital area of study as we begin to unravel the complexities of neurodegeneration. By understanding the role of the immune system in neurodegenerative diseases, researchers can develop targeted therapies that address the root causes of conditions like Alzheimer’s. As investigators explore immune checkpoints such as TIM-3, the potential to create therapies that effectively combat the disease is within reach, highlighting the importance of interdisciplinary collaboration.
In examining the relationship between immune dysregulation and Alzheimer’s progression, the research highlights the critical nature of the immune response in maintaining neural integrity. Investigating how immune checkpoints can be manipulated offers promising avenues for therapeutic development. By focusing on targeted treatments that can enhance immune recognition and clearance activities within the brain, researchers aim to leverage the body’s own defenses to combat Alzheimer’s, paving the way for novel strategies in both research and clinical applications.
Frequently Asked Questions
How does TIM-3 relate to Alzheimer’s treatment?
TIM-3, an immune checkpoint molecule, has shown potential in Alzheimer’s treatment by inhibiting microglial cells from clearing plaques in the brain. Recent research indicates that deleting TIM-3 expression can enhance the ability of these immune cells to attack and remove amyloid plaques, thereby improving cognitive function.
What are the implications of TIM-3 in Alzheimer’s research?
TIM-3 has emerged as a critical focus in Alzheimer’s research due to its role in regulating the immune response in the brain. Studies suggest that TIM-3’s inhibitory effect on microglia contributes to plaque accumulation in Alzheimer’s disease, highlighting it as a target for therapeutic intervention.
How does the immune system and Alzheimer’s relate to TIM-3?
The immune system’s regulation via TIM-3 is vital in Alzheimer’s disease, as this checkpoint molecule prevents microglia from effectively removing harmful plaques. By understanding TIM-3’s function, researchers aim to develop treatments that could reverse cognitive decline by enhancing the immune system’s response.
Can cancer treatment strategies involving TIM-3 be applied to Alzheimer’s disease?
Yes, cancer treatment strategies that target TIM-3 are being explored in Alzheimer’s disease. By repurposing anti-TIM-3 antibodies that have been effective in oncology, researchers hope to develop therapies that can improve microglial function and reduce plaque formation in the brain.
What role do microglia play in Alzheimer’s disease regarding TIM-3?
Microglia are the primary immune cells in the brain, crucial for maintaining brain health by pruning synapses and clearing debris. In Alzheimer’s, TIM-3 expression on microglia hinders their ability to clear amyloid-beta plaques, leading to further brain damage and cognitive decline.
What are the next steps in TIM-3 Alzheimer’s treatment research?
Researchers are currently investigating whether human anti-TIM-3 antibodies can effectively halt plaque formation in Alzheimer’s disease mouse models. These studies aim to confirm the therapeutic potential of targeting TIM-3 to enhance brain immunity against amyloid plaques.
How does TIM-3 affect cognitive function in Alzheimer’s disease models?
By genetically deleting TIM-3 in mouse models of Alzheimer’s, researchers observed improved cognitive function. These mice exhibited enhanced memory and learning capabilities, suggesting that targeting TIM-3 can restore normal microglial function and mitigate the effects of Alzheimer’s-related plaque accumulation.
What findings were published regarding TIM-3 and Alzheimer’s in recent research?
Recent findings published in “Nature” highlight that TIM-3 deletion allows microglia to regain their function in clearing plaques, leading to significant improvements in memory and cognitive behaviors in mouse models of Alzheimer’s disease, thereby offering insights into potential treatment pathways.
Is there a genetic link between TIM-3 and Alzheimer’s disease?
Yes, studies indicate that a polymorphism in the TIM-3 gene is associated with an increased risk of late-onset Alzheimer’s disease, suggesting a genetic predisposition connected to the immune response in the development of the disease.
What does therapy targeting TIM-3 for Alzheimer’s look like?
Therapies targeting TIM-3 for Alzheimer’s could involve anti-TIM-3 antibodies or small molecules designed to block the inhibitory effects of TIM-3, potentially allowing microglia to better tackle amyloid plaques and improve cognitive outcomes in affected individuals.
| Key Points | Details |
|---|---|
| Research Focus | Explores the potential of TIM-3 as a therapeutic target for Alzheimer’s treatment. |
| Study Findings | Deleting TIM-3 allows microglia to clear amyloid plaques and improves cognitive function in mice. |
| TIM-3 Role | TIM-3 inhibits microglia’s ability to remove harmful plaques in the brain, contributing to Alzheimer’s pathology. |
| Clinical Implication | Possibility of using TIM-3 antibodies in therapies to enhance plaque clearance in Alzheimer’s patients. |
| Research Collaboration | Conducted in collaboration between genetic and immunological expert laboratories at Harvard. |
Summary
TIM-3 Alzheimer’s treatment represents a groundbreaking approach where modifying the TIM-3 checkpoint molecule allows brain immune cells to effectively tackle amyloid plaques, which are central to the disease. This innovative method has shown promising results in mice, indicating a potential pathway for future human therapies aimed at enhancing memory and cognitive function in Alzheimer’s patients. As research evolves, leveraging TIM-3 could transform the treatment landscape for Alzheimer’s disease, offering hope for improved patient outcomes.