Pediatric Cancer Prediction: AI Outperforms Traditional Methods
Pediatric cancer prediction is rapidly evolving, especially with the integration of artificial intelligence in pediatric oncology. Recent studies have shown that AI tools can significantly enhance the accuracy of predicting brain tumor recurrence, focusing on pediatric gliomas. By employing advanced methodologies like temporal learning, researchers can analyze multiple brain scans over time, creating a nuanced picture of a child’s potential relapse risk. This is a game-changer for pediatric glioma treatment, as it allows for more personalized care strategies and reduces the anxiety associated with frequent imaging. As we refine these predictive models, we are moving closer to better outcomes for children battling these challenging conditions.
The forecasting of cancer relapse in young patients, particularly in the context of brain tumors, represents a significant advancement in pediatric healthcare. By utilizing innovative technologies in pediatric oncology, medical professionals are gaining fresh insights into glioma relapse prediction. This new focus on temporal learning offers a promising avenue for understanding brain tumor recurrence risk, leading to improved pediatric glioma treatment strategies. Furthermore, these advancements show potential for reshaping how we approach the monitoring and management of pediatric cancer, providing a beacon of hope for families navigating this difficult journey. As AI continues to evolve, its applications could revolutionize care for this vulnerable population.
Understanding Pediatric Cancer Prediction
Pediatric cancer prediction, particularly for brain tumors, has seen significant advancements thanks to artificial intelligence (AI). Traditionally, predicting the risk of recurrence in pediatric gliomas relied on periodic imaging and clinical assessments. However, these methods often fell short in accurately identifying high-risk patients. The introduction of AI technologies, especially those utilizing temporal learning, marks a transformative shift in how oncologists evaluate the likelihood of cancer recurrence. By analyzing sequential brain scans over time, these AI models can detect patterns that are otherwise imperceptible to human observers.
The predictive capabilities offered by AI in pediatric oncology enable more tailored treatment plans, helping healthcare professionals identify which patients may need more aggressive follow-up or intervention. The studies have shown that AI tools can outpace traditional prediction methods in accuracy, which is crucial for diseases like gliomas where timely intervention can significantly improve outcomes. Early and reliable identification of patients at high risk can lead to reduce stress on families, while potentially decreasing the frequency of unnecessary imaging procedures.
The Role of AI in Pediatric Oncology
Artificial Intelligence is reshaping pediatric oncology by offering innovative solutions for complex predictive problems. In this era of technological advancement, AI tools are being developed to analyze vast datasets, including imaging data, to discern intricate patterns related to cancer progression. For instance, in pediatric glioma cases, AI can process thousands of MRI scans, identifying subtle changes over time that may indicate a risk of relapse. This capability not only enhances the accuracy of risk assessments but also facilitates personalized treatment approaches for young patients.
Moreover, AI in pediatric oncology does not merely assist in recognizing potential relapse but also holds promise in optimizing treatment protocols. With the integration of predictive AI tools, oncologists can make informed decisions on the necessity of preventive therapies for high-risk patients. This proactive stance enhances not only the safety and efficacy of treatment options but also minimizes the emotional and financial burden on families, paving the way for a more supportive healthcare environment.
Temporal Learning Techniques in Medical Imaging
Temporal learning is a groundbreaking approach that boosts the predictive power of AI models in medical imaging, particularly in the field of oncology. This method entails training AI systems to analyze consecutive imaging data from a single patient to understand how tumors behave over time. With gliomas being a focus area, temporal learning allows for the sophisticated assessment of tumor dynamics that traditional analyses may overlook. This approach yields a more holistic view of tumor development, vastly improving the accuracy of relapse predictions.
By utilizing temporal learning, researchers can turn sequential MR scans into a narrative of the tumor’s evolution, leading to better-informed clinical decisions. The ability to track changes over time not only enhances understanding but also equips clinicians with the tools necessary for timely interventions. Given the significant implications for pediatric patients facing glioma treatments, this technology promises not only to make cancer predictions more reliable but also to transform the trajectory of care in pediatric oncology.
AI-Enhanced Predictions for Glioma Relapse Risk
Predicting glioma relapse risk has taken a giant leap forward with the introduction of AI-driven methodologies. Prior attempts at predicting outcomes were often limited by their reliance on static imaging data, which failed to provide a comprehensive view of tumor behavior. However, the recent integration of advanced AI tools allows researchers to leverage multiple scans taken over time, dramatically improving prediction outcomes. Through rigorous training, these AI systems can distinguish between low and high-grade gliomas, providing clinicians with critical insights into each patient’s specific risk profile.
The implications of enhanced glioma relapse predictions extend far beyond individual patient care. By accurately determining relapse potential, oncologists can develop more effective long-term management strategies tailored to each patient’s unique situation. This optimization could involve minimizing unnecessary MRIs for patients deemed low-risk while ensuring that those identified as high-risk receive immediate and targeted interventions. Ultimately, this paradigm shift, driven by AI technology, represents a significant advancement in pediatric cancer care, leading to improved outcomes and comprehensive support systems for young patients and their families.
Improving Pediatric Glioma Treatment Outcomes
The treatment landscape for pediatric gliomas is undergoing a transformative change, thanks in large part to AI innovations and advanced predictive models. These technologies are equipping healthcare providers with the ability to identify which children might be at higher risk of experiencing recurrence following initial treatment. By fine-tuning treatment plans based on robust AI predictions, healthcare professionals can tailor interventions, ensuring that patients receive the most effective care possible. This shift towards personalized treatment is expected to lead to improved long-term outcomes for children battling these challenging tumors.
Moreover, the insights generated from AI analytics support a proactive management approach towards pediatric glioma care. By determining the likelihood of relapse with greater accuracy, oncologists can implement strategic follow-up plans, reducing the anxiety associated with frequent imaging and allowing families to focus more on quality of life. As research continues to evolve, the integration of these AI-driven methodologies within clinical settings promises to revolutionize how pediatric gliomas are treated and monitored, heralding a new era of enhanced pediatric oncology.
The Future of AI in Pediatric Oncology Research
The future of AI in pediatric oncology research is brimming with potential, especially as more studies showcase its effectiveness in improving patient outcomes. With ongoing advancements in machine learning and data analysis, AI systems are expected to become increasingly sophisticated in their predictive capabilities. The continued exploration of AI applications, such as those focusing on gliomas and other pediatric cancers, is likely to unveil new insights into disease progression and management. As these technologies are refined, they pave the way for groundbreaking clinical trials and research initiatives, potentially altering the standard of care for pediatric oncology.
Furthermore, there is a growing need for collaborations between researchers, clinicians, and technology experts to harness the full potential of AI. By ensuring that AI tools are developed with clinical relevance and patient needs in mind, the oncology community can ensure these innovations translate seamlessly into practice. The ultimate goal remains clear: to improve the lives of pediatric cancer patients by predicting their treatment trajectories accurately and providing personalized care strategies that maximize their chances of long-term survival and quality of life.
Reducing Imaging Frequency Through Predictive Analytics
One of the key benefits of employing AI in pediatric oncology is the potential to significantly reduce imaging frequencies for patients identified as low-risk. Traditional follow-up protocols often involved frequent MRIs, which could be both invasive and emotionally taxing for young patients and their families. However, AI’s ability to accurately predict the likelihood of relapse means that oncologists can move towards a model of tailored follow-ups. By relying on robust AI analyses, healthcare providers can maximize screening efficiency while minimizing unnecessary procedures.
This shift is not only beneficial for the patients but also helps alleviate the burden on healthcare systems. Fewer imaging sessions mean reduced costs and resource allocation, allowing medical teams to focus on more critical care needs. As predictive analytics continue to evolve, creating more precise risk stratification models for pediatric glioma patients, the integration of AI into follow-up routines will undoubtedly result in more humane, cost-effective, and patient-centered care.
Ethical Considerations in AI-Driven Pediatric Oncology
While the benefits of AI in pediatric oncology are substantial, there are also critical ethical considerations to address. The application of AI tools in predicting pediatric cancer recurrence raises questions about data privacy, the accuracy of predictions, and the decision-making processes involved. As AI systems become integral to patient management, ensuring that families understand and consent to how their data will be used is paramount. Moreover, ethical guidelines must be established to prevent biases in AI predictions that could disproportionately affect certain groups of patients.
Additionally, as clinical trials begin to implement AI-enhanced predictions, it’s essential for the research community to establish transparent protocols that prioritize patient welfare. Assessing and validating AI tools in diverse healthcare environments is required to ensure equitable access to improved predictive models. In embracing AI for pediatric oncology, stakeholders must remain vigilant about ethical standards, ensuring that advancements deliver equitable benefits to all individuals and nurture the trust required for effective healthcare delivery.
Potential of AI in Early Detection of Pediatric Brain Tumors
The potential of AI in the early detection of pediatric brain tumors represents one of the most promising aspects of integrating technology into oncology. Leveraging machine learning algorithms that analyze imaging data can enable clinicians to detect minute changes indicative of tumors much earlier than traditional methods allow. Early detection is critical, particularly in the case of pediatric gliomas, where prognosis significantly improves with timely intervention. Thus, harnessing AI technologies to support early diagnosis could revolutionize treatment pathways for many children.
In addition to enhancing diagnostic accuracy, AI’s role in early detection carries the potential to shape preventive strategies in pediatric oncology. By identifying at-risk patients early, healthcare providers can implement regular monitoring and proactive treatments to lower the chances of severe outcomes. As research and development in this field advance, the collaborative efforts across institutions will likely yield AI tools that enhance not only early detection but also comprehensive care solutions for young patients battling brain tumors.
Frequently Asked Questions
What is pediatric cancer prediction and how does it relate to AI in pediatric oncology?
Pediatric cancer prediction refers to the use of advanced technologies, including machine learning and AI, to forecast the likelihood of cancer recurrence in children. In pediatric oncology, AI tools analyze various data points, including imaging and clinical history, to improve predictions regarding conditions like glioma. By leveraging AI, healthcare providers can enhance early detection and management strategies for pediatric cancer patients.
How is glioma relapse prediction improved by AI tools?
AI tools enhance glioma relapse prediction by analyzing multiple MRI scans of pediatric patients over time using a method called temporal learning. This approach allows AI to track subtle changes in the brain scans, making it significantly more accurate in predicting relapse compared to traditional single-scan methods.
What role does temporal learning in medicine play in pediatric cancer prediction?
Temporal learning plays a crucial role in pediatric cancer prediction by allowing AI algorithms to learn and interpret trends and changes across multiple patient scans taken over time. This technique improves the model’s accuracy in predicting outcomes, like glioma recurrence, by incorporating the progression of imaging data, rather than relying on isolated scans.
What are the benefits of accurately predicting brain tumor recurrence risk in children?
Accurate prediction of brain tumor recurrence risk in children leads to better personalized treatment plans and reduces unnecessary follow-up imaging. With precise predictions, healthcare providers can allocate resources efficiently, ensure optimal monitoring for high-risk patients, and potentially initiate preventive therapies for those at greater risk of recurrence.
How does AI improve pediatric glioma treatment strategies?
AI improves pediatric glioma treatment strategies by enabling healthcare providers to better predict which patients are at high risk for cancer recurrence. This allows for more tailored treatment approaches, potentially reducing the frequency of imaging and informing the need for adjuvant therapies, ultimately leading to improved patient outcomes.
What findings were revealed in the recent AI study on pediatric gliomas?
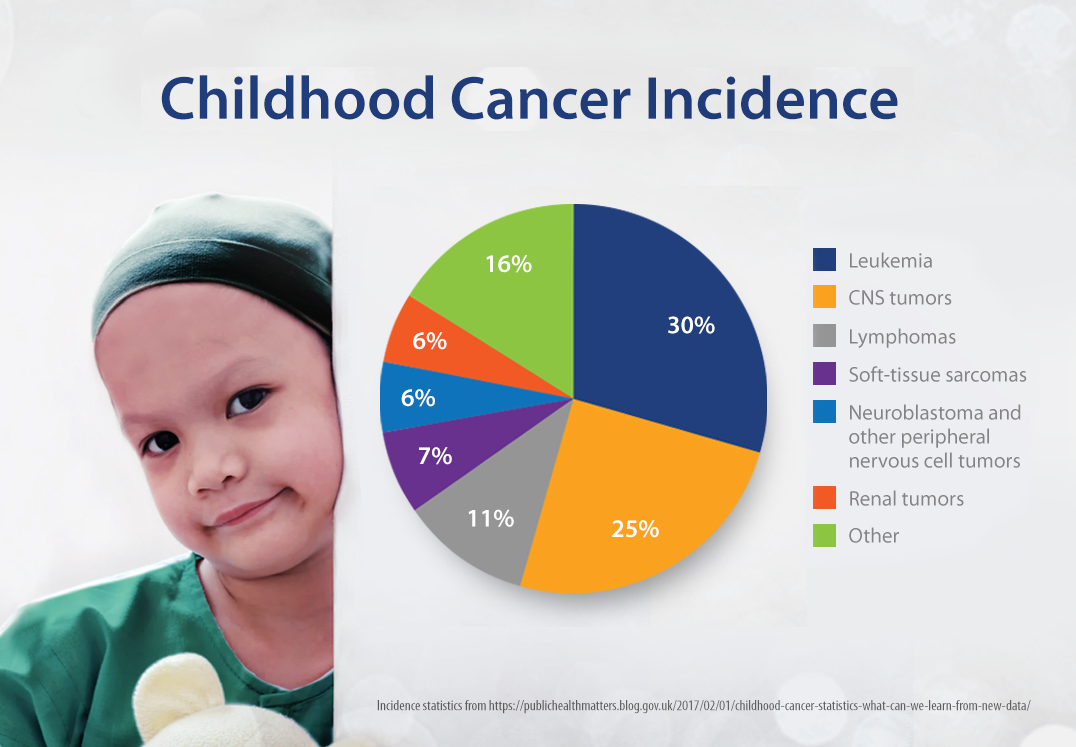
The recent study highlighted that the AI model using temporal learning could accurately predict recurrence of pediatric gliomas within one year post-treatment, achieving an accuracy rate of 75-89%. This was a significant improvement over traditional methods, which had an accuracy of about 50%, demonstrating the potential of AI in enhancing pediatric cancer prediction.
What are the next steps following the research on AI in pediatric oncology?
Following this research, the next steps include conducting clinical trials to validate the AI model’s predictions in real-world settings. Researchers aim to determine if these AI-informed insights can improve care protocols for pediatric glioma patients and possibly lead to advancements in treatment options.
| Key Point | Details |
|---|---|
| AI Tool for Predictions | An advanced AI tool predicts relapse risk in pediatric cancer patients more accurately than traditional methods. |
| Study Overview | Conducted by researchers from Mass General Brigham, Boston Children’s Hospital, and others, the study used nearly 4,000 MR scans from 715 patients. |
| Temporal Learning | This technique synthesizes findings from multiple brain scans over time, improving prediction of cancer recurrence. |
| Prediction Accuracy | The temporal learning model predicts recurrence with 75-89% accuracy, significantly better than the 50% accuracy of single images. |
| Potential Benefits | Improved risk prediction could lead to tailored treatment plans and reduced imaging frequency for low-risk patients. |
| Future Directions | Further validation and clinical trials are necessary to implement AI-informed predictions in clinical settings. |
Summary
Pediatric cancer prediction has witnessed significant advancements with the introduction of AI tools capable of accurately forecasting cancer recurrence risk. By utilizing advanced techniques like temporal learning and analyzing multiple brain scans over time, researchers have made strides in enhancing prediction accuracy. This innovative approach aims to improve patient care by reducing unnecessary stress for families and optimizing treatment strategies for pediatric glioma patients.