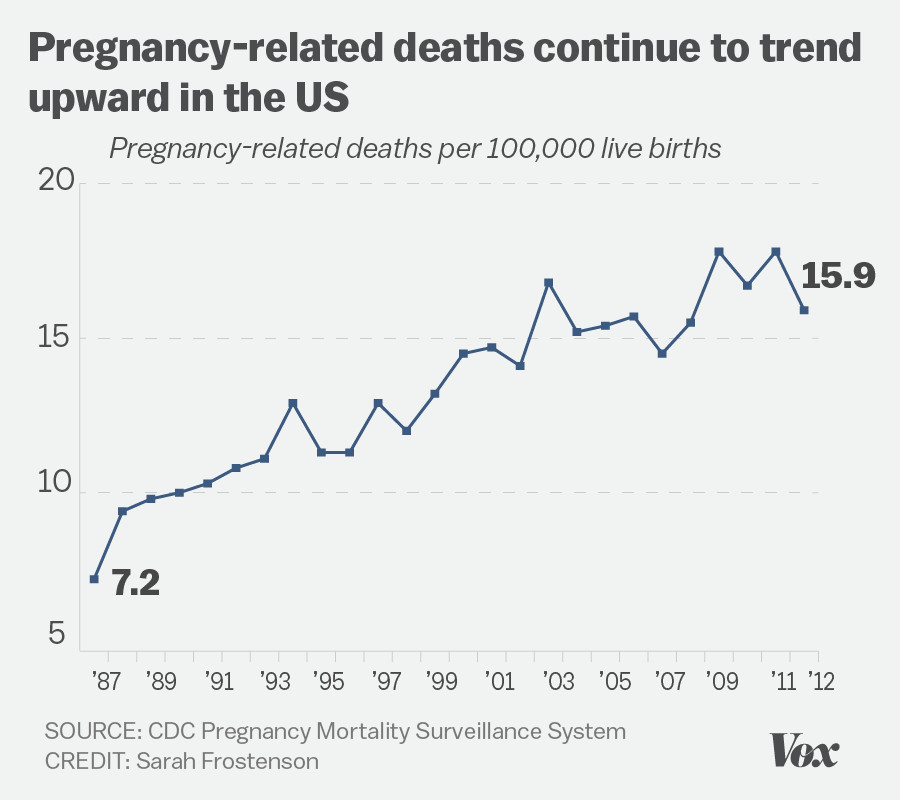
U.S. pregnancy-related deaths are alarmingly on the rise, marking a troubling trend that sets the nation apart as a leader in maternal mortality among high-income countries. Despite over 80% of these fatalities being preventable, systemic issues in pregnancy care contribute significantly to this crisis. A recent CDC pregnancy study highlights just how disparities in access to health services impact outcomes for mothers across various demographics. With staggering statistics showing that American Indian and Alaska Native women experience nearly four times the mortality rate of white women, these health disparities underscore the urgent need for improved maternal and postpartum care. As we delve into this critical issue, it becomes clear that addressing the complexities of maternal health is paramount to safeguarding the lives of future generations.
The rising number of maternal deaths in the United States highlights a significant public health challenge that merits urgent attention. Health experts emphasize the need for enhanced pregnancy management and ongoing postpartum support to tackle the underlying issues fueling this escalation. Various factors contribute to the increasing rates, including chronic health conditions among expectant mothers and inequitable healthcare access. The urgency of the situation calls for comprehensive approaches that address disparities in maternal health outcomes, particularly among marginalized communities. As we explore the dynamics of this health crisis, it becomes apparent that a transformative response is essential for improving the overall health of mothers and their infants alike.
Understanding U.S. Pregnancy-Related Deaths
In the U.S., the alarming rise in pregnancy-related deaths highlights a significant public health crisis that needs urgent attention. A recent study reveals that over 80 percent of these deaths are preventable, yet the U.S. remains at the forefront of maternal mortality rates among high-income countries. The systemic issues underlying these figures are multifaceted, including inadequate prenatal care, variations in healthcare access, and a lack of postpartum support that neglects the long-term health of new mothers. Addressing these gaps in care is critical to preventing further fatalities.
Data from the CDC shows that pregnancy-related deaths continued to climb between 2018 and 2022, with the most notable increase occurring during the COVID-19 pandemic. These trends expose the stark realities of health disparities experiencing populations where maternal mortality rates are disproportionately high among American Indian and Alaska Native women as well as non-Hispanic Black women. The need for targeted interventions that ensure equitable resources and care for all racial and ethnic groups is paramount for reversing this trend.
The Impact of Health Disparities on Maternal Mortality
Health disparities significantly affect maternal mortality rates in the U.S., creating a troubling reality where factors such as race, ethnicity, and geographical location play a pivotal role in determining outcomes for mothers. States with inadequate healthcare infrastructure are more likely to report higher rates of pregnancy-related deaths. For example, while California has made notable strides in reducing its maternal mortality rate, other states still grapple with troubling statistics. Such inconsistencies highlight the importance of implementing comprehensive policies that address the diverse needs of expectant mothers and ensure consistent access to high-quality pregnancy care across the country.
Moreover, biases present within the healthcare system contribute to these health disparities. Discrimination can manifest in various ways, leading to a lack of trust in health services from underrepresented groups, ultimately affecting their willingness to seek care during pregnancy. To combat these challenges, healthcare providers must receive training that emphasizes cultural competency, improving engagement with all patients, and ensuring that their experiences and concerns are addressed sufficiently.
The Importance of Extended Postpartum Care
Extended postpartum care has emerged as a critical component in the fight against maternal mortality in the U.S. The conventional understanding of postpartum care often terminates 6 weeks after delivery, but new evidence underscores the importance of ongoing support for up to a year after childbirth. Late maternal deaths, which occur from 42 days to one year postpartum, account for nearly a third of all maternal deaths, emphasizing the urgent need to redefine postpartum care to support women’s health more comprehensively during this period.
Investing in innovative postpartum programs can facilitate better mental and physical health outcomes for mothers. These programs may include follow-up visits that monitor chronic conditions such as hypertension, nutritional support, and mental health resources addressing postpartum depression. A holistic approach ensures mothers receive appropriate medical care throughout the first year of motherhood, which is essential for both maternal and infant health alike.
Innovations Needed in Pregnancy Care Systems
With the rising rates of maternal mortality, there is an urgent call for innovations in pregnancy care systems to enhance maternal health outcomes. The CDC pregnancy study highlights various successes in states like California, suggesting that adopting similar policies in underperforming states could prevent thousands of pregnancy-related deaths. Innovations could involve improving telehealth services for prenatal appointments, ensuring consistent access to specialists for at-risk mothers, and investing in community health initiatives that provide comprehensive education about pregnancy care.
Additionally, health systems must prioritize data collection and research to better understand maternal mortality trends. By analyzing the factors contributing to pregnancy-related deaths, policymakers can implement targeted solutions. Enhancing the infrastructure for tracking these events is essential, as accurate data allows for informed decisions regarding funding and resources for maternal health initiatives.
The Role of Public Health Infrastructure in Maternal Health
Public health infrastructure is vital to addressing the rising rates of pregnancy-related deaths in the U.S. Investing in this infrastructure can facilitate better tracking of maternal mortality, provide funding for innovative care models, and ensure that resources are allocated effectively where they are needed most. A strong public health system is essential to collecting accurate data on maternal health trends, which in turn informs policymakers and advocates striving for change.
Moreover, a robust public health approach promotes real-time adjustments to healthcare policies, ultimately aligning them with the evolving needs of mothers across the country. As funding cuts threaten public health initiatives, sustained investment is crucial to reversing the trend of climbing maternal mortality rates and moving towards a future where every mother can enjoy a safe and healthy pregnancy.
Addressing Racial and Ethnic Disparities in Maternal Health
Racial and ethnic disparities in maternal health are significant challenges that need addressing to reverse the upward trend in pregnancy-related deaths. For instance, American Indian and Alaska Native women experience significantly higher mortality rates compared to their white counterparts, indicating systemic failings within healthcare access and treatment. Healthcare systems must recognize these disparities and take actionable steps to develop culturally sensitive policies aimed at improving outcomes for marginalized groups.
Implementing community-based programs that empower women of color through education, support networks, and healthcare advocacy can promote better prenatal and postpartum outcomes. Such initiatives not only educate expectant mothers about their health but also engage them in meaningful dialogues with healthcare providers, fostering relationships built on trust and respect.
The Importance of Maternity Care Access
Access to quality maternity care is foundational for ensuring the health and safety of both mothers and infants. The U.S. faces a patchwork healthcare system where many women lack access to comprehensive prenatal and postpartum services, leading to increased risks during and after pregnancy. Maternity care deserts, particularly in rural areas, exacerbate this issue, as women are forced to travel long distances for essential services.
To improve access, policymakers must prioritize the development of transportation services and telemedicine options that can eliminate barriers for expectant mothers in underserved regions. Additionally, ensuring that healthcare providers are distributed equitably across all demographics will improve maternal health outcomes and help reduce the maternal mortality rates that plague the nation.
Combating Chronic Conditions in Pregnant Women
Chronic health conditions, including obesity and hypertension, have shown alarming increases among women of reproductive age and pose significant risks during pregnancy. As cardiovascular disease becomes the leading cause of pregnancy-related death, it is crucial for healthcare professionals to focus on managing these chronic conditions effectively before, during, and after pregnancy. This may involve personalized care plans that address the specific health needs of each individual.
Addressing these chronic health issues necessitates education and intervention strategies tailored toward prevention, early detection, and management. Health professionals should regularly screen for risks before conception and provide guidance on lifestyle modifications to improve health outcomes. By proactively engaging with women regarding their health, the cycle of chronic disease affecting maternal mortality can be disrupted.
The Need for Comprehensive Education in Pregnancy Care
Comprehensive education on pregnancy care is essential for preventing maternal mortality. Many women are unaware of the signs and risks associated with pregnancy-related complications, which can lead to delayed emergency responses. Healthcare providers should prioritize educating patients about the warning signs of pregnancy emergencies and the importance of seeking timely care.
In addition, educational efforts should extend to discussions on postpartum care, including mental health resources. Many women experience significant challenges after childbirth, yet they often feel isolated in their struggles. Programs that provide information about postpartum depression and support can help women navigate this critical period, ultimately improving outcomes for mothers and their families.
Frequently Asked Questions
What are the main causes of U.S. pregnancy-related deaths?
In the U.S., the leading causes of pregnancy-related deaths include cardiovascular disease, hemorrhage, and infections. Between 2018 and 2022, cardiovascular disease accounted for over 20% of such deaths, reflecting an alarming increase in chronic conditions affecting pregnant individuals. Addressing these causes is essential to reduce maternal mortality rates.
How do health disparities impact U.S. pregnancy-related deaths?
Health disparities significantly impact U.S. pregnancy-related deaths, with racial groups experiencing markedly different outcomes. American Indian and Alaska Native women show the highest mortality rates, while non-Hispanic Black women also face substantial risks. These disparities are rooted in systemic biases, access to quality care, and social determinants of health.
How does postpartum care relate to U.S. pregnancy-related deaths?
Postpartum care is crucial in addressing U.S. pregnancy-related deaths, particularly since nearly one-third of maternal deaths occur between 42 days and one year after pregnancy. Improving care during this extended postpartum period can help reduce mortality rates and ensure women receive necessary support for recovery.
What role does the CDC play in tracking U.S. pregnancy-related deaths?
The CDC plays an essential role in tracking U.S. pregnancy-related deaths through national data collection and research initiatives. Their studies help identify trends, causes, and disparities in maternal mortality, guiding public health policies to improve pregnancy care and health outcomes for mothers.
Why are U.S. pregnancy-related death rates continuing to rise?
U.S. pregnancy-related death rates continue to rise due to factors such as inequitable healthcare access, increasing rates of chronic health issues, and systemic biases within the healthcare system. Addressing these underlying factors is critical for stopping the rise in maternal mortality.
What steps can be taken to reduce U.S. pregnancy-related deaths?
To reduce U.S. pregnancy-related deaths, it is vital to invest in comprehensive prenatal and postpartum care, improve access to quality healthcare, address social determinants of health, and implement evidence-based policies that target health disparities experienced by different racial and ethnic groups.
How does the high rate of maternal mortality in the U.S. compare to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income countries, with significant disparities across states and racial groups. This stark contrast indicates a need for systemic improvements in pregnancy and postpartum care to align the U.S. with international standards.
What are ‘late maternal deaths’ and why are they significant?
‘Late maternal deaths’ refer to deaths that occur between 42 days and one year after pregnancy. They are significant because they highlight the need for comprehensive postpartum care, as many deaths in this period could be prevented with improved health systems and continuous support beyond the immediate postpartum phase.
| Key Point | Details |
|---|---|
| Rising Rates of U.S. Pregnancy-Related Deaths | The U.S. has the highest maternal mortality rate among high-income countries, which has continued to rise from 2018 to 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths in the U.S. are preventable, indicating a need for better healthcare and policies. |
| Disparities by Race and Ethnicity | There are significant racial disparities, with American Indian and Alaska Native women having the highest mortality rate. |
| Impact of COVID-19 | The sharpest increase in pregnancy-related deaths occurred in 2021, likely due to the COVID-19 pandemic. |
| Need for Improved Care | To reduce pregnancy-related deaths, the U.S. must enhance prenatal and postpartum care and address systemic inequalities. |
| Late Maternal Deaths | Late maternal deaths, occurring beyond 42 days postpartum, accounted for nearly a third of total deaths. |
Summary
U.S. pregnancy-related deaths are a growing public health crisis that call for immediate attention and action. Despite the potential to prevent over 80% of these deaths, systemic healthcare issues, disparities by race, and the impacts of the COVID-19 pandemic have exacerbated maternal mortality. To improve outcomes, significant investment in healthcare infrastructure and a focus on equitable, continuous care throughout the prenatal and postpartum periods are essential. Addressing these factors is crucial for effectively reducing U.S. pregnancy-related deaths and ensuring better maternal health for all.